Published: May 03, 2024
Authors: Natan Bar-Chama, Lev Rabinovitch, Stanton Honig
DOI: https://doi.org/10.1016/j.urology.2024.04.001
Original Article: https://www.goldjournal.net/article/S0090-4295(24)00257-7/fulltext
Objective
To assess the accuracy of the YO home sperm test by real-world/amateur users.
Methods
This multisite study investigated whether amateur users could use the FDA-cleared YO Home Sperm Test to obtain accurate motile sperm concentration (MSC) results when compared to trained laboratory technicians. The qualitative MSC results of amateur and professional YO users were compared to each other as well as to the results of an established automated sperm quality analyzer (SQA-V) above and below a 6 m/mL MSC cut-off.
Results
This was a blinded, prospective study of 316 amateur users and 3 professional laboratory technicians across 3 study sites. Amateur vs Professional YO users demonstrated an accuracy of >97%. Qualitative results of amateurs and professionals vs SQA-V results showed a >95.7% accuracy.
Conclusion
Amateur users with no prior training were able to follow the YO test directions to receive highly accurate qualitative motile sperm concentration (MSC) results. The YO test is user-friendly and can be used as an effective initial home screening tool to gain preliminary insight into the fertility status of the male in a real-world setting. Furthermore, the YO test results correlated with those obtained by the FDA-cleared SQA-V laboratory analyzer, confirming that the YO test delivers accurate MSC results in the hands of amateur users.
Infertility is a medical disease of the male or female reproductive system defined by the failure to achieve a pregnancy after 12 months or more of regular unprotected sexual intercourse. Infertility affects 1 in 5 couples, and of these, 40%-50% have a male contributing factor.1
While a full fertility work-up might be initiated for the female by her obstetrician/gynecologist, this same physician may not have the relevant training or capacity to assess the fertility of the male partner. Unfortunately, this reality may impact compliance with the most recently published AUA/ASRM guidelines (2021), recognizing that an infertile couple should, from the outset, undergo a concurrent assessment.3
Although semen analysis is a noninvasive and relatively simple diagnostic test, concerned couples may wait for a year or more before a fertility workup is initiated or funded by their health provider. Moreover, men may resist testing because of embarrassment, or feel intimidated by the public nature of providing an ejaculate in a doctor’s office or laboratory setting.4
Furthermore, the psychological barrier to undergoing a semen analysis is multifaceted and the male partner may see his fertility as integral to his perception of self, underscoring both his role in procreation and his overall virility or “manliness.” In the presence of male factor infertility, a couple’s path to pregnancy may be prolonged due to the male partner’s reluctance to undergo testing. Delays can be detrimental, particularly in the presence of advancing female age or diminished ovarian reserve. Consequently, there is value in encouraging men to test their sperm quality early in the family-building journey, and a user-friendly male home fertility test could facilitate the male partner to test himself early on.
Home testing is not a new phenomenon, and the utilization and acceptance of remote medical encounters and screening have been accelerated by the COVID-19 pandemic. The development of new, connected e-health technology platforms has received increasing global attention, technological enhancements, and acceptance. In fact, the latest WHO 6th edition guidelines for semen analysis state that computer-aided sperm analysis and additional technologies, including smartphone-based devices, have great potential for sperm analysis in producing reliable and reproducible results. While Smartphone-based tests may not yet achieve the accuracy required for medical acceptance, it is noted that the use of these devices “could become a useful means for men to seek early proper medical advice, investigation, and causal treatment.”5
For a Smartphone “over the counter” device to successfully obtain FDA clearance, it must demonstrate the ability to provide accurate results in the hands of an untrained user in the home environment. Clear and detailed instructions are therefore required to guide an amateur user to perform a complex test such as semen analysis. The YO Home Sperm Test was the first Smartphone-based male fertility screening device to receive FDA clearance. It is uniquely positioned in that it differentiates itself from other FDA-approved over-the-counter male fertility testing options by assessing an integrated sperm motility/concentration parameter reported as motile sperm concentration (MSC), live video capture of the sample and a YO Score grading classification.6
The purpose of this study is to establish the real-world experience of the YO Home Sperm Test (“YO test” or “YO device”) in terms of accuracy and overall usability in the hands of a large population of demographically diverse, untrained users.
MATERIALS AND METHODS
The primary objective of this study was to investigate whether a diverse population of real-world amateur users could readily use the YO Home Sperm Test (YO) to obtain accurate MSC results vs professionally trained laboratory technicians. Sperm donors at each study site were recruited as amateurs for the study. 316 amateurs were consented, and the study was conducted under an IRB-approved protocol. This blinded prospective study was conducted at Xytex Sperm Bank, Augusta, Georgia (82 participants); Xytex Sperm Bank, New Brunswick, New Jersey (136 participants); Medical Electronic Systems, Caesarea, Israel (98 participants). Each of the three study sites had its own professional laboratory technician (3 professionals) who were trained in performing analysis on both the YO device and the SQA-V automated semen analyzer.
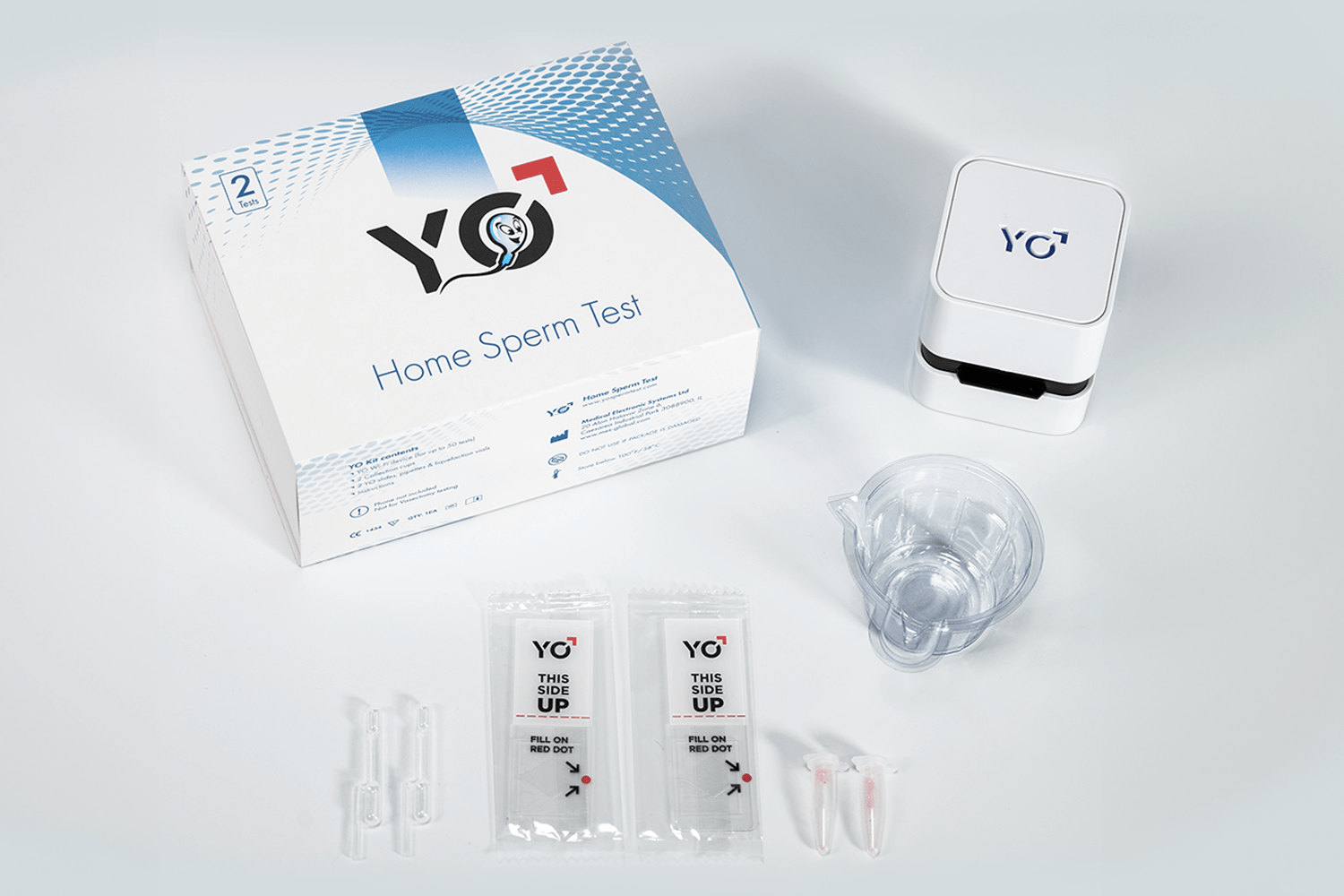
The YO Home Sperm Test (Medical Electronic Systems, FDA cleared – K161493), is a class 2 smartphone-based medical device. In combination with the YO app, it captures a video of a semen sample and performs a qualitative assessment of MSC. MSC is an integrated sperm parameter derived from multiplying sperm concentration and percent motility. The YO test reports whether a user’s MSC is above or below a cut-off of 6 million motile sperm per mL (6 m/mL). The YO MSC cut-off is derived from the WHO 5th edition reference cutoff for sperm concentration (15 million per mL) multiplied by the reference cutoff for sperm motility (40%). The YO test discriminates between the low MSC below the cutoff (<6 million/mL) and moderate/normal MSC above the cutoff (≥6 m/mL).6, 7, 8, 9, 10, 11, 12
The SQA-V automatic semen analyzer (Medical Electronic Systems, FDA cleared – K012352) was selected as the comparative device to the YO Home Sperm Test. The SQA-V automatic semen analyzer was validated vs manual semen analysis in several parameters including concentration, motility, and morphology. It was also concluded that the SQA-V used for routine semen analysis within the andrology laboratory setting improved efficiency and precision as well as positively impacted standardization protocols.13, 14
The SQA-V automatic semen analyzer measures MSC, provides automatic results in approximately 2 minutes, and is accepted and routinely used by numerous commercial laboratory chains and andrology facilities in the USA and throughout the world.
The focused diversity of the amateur cohort offered confidence that the likely usability of the YO test within the actual population could be ascertained, regardless of cultural background, age, level of education, and familiarity with fertility or other medical issues. Of the 316 amateurs, 292 male participants tested their own semen sample. The remaining 24 female participants, who were without intimate partners, tested donor semen samples with the YO device. In parallel one trained professional at each of the three study sites conducted blinded testing on the YO and the comparator SQA-V device.
Each amateur selected either an Apple iPhone or a Samsung Galaxy Smartphone to run their YO test. All testing supplies included in the YO kit were provided to amateur users. Testing was performed by the amateur without coaching, following only the step-by-step instructions in the YO app and the YO product insert. The YO user interface provides training videos and onscreen step-by-step instructions of the testing process. The testing steps included: Sample liquefaction and mixing, slide filling and insertion into the YO device, and initiating sample analysis.
Male participants collected their own semen samples following instructions based on the sample handling guidelines of the WHO laboratory manual for the examination and processing of human semen.7
Female participants ran donor samples. All samples were split into two aliquots, one tested on a YO device by an amateur, and in parallel the laboratory professional conducted aliquot 2 testing on the SQA-V and YO device using the same phone model and batch number of testing supplies as the amateur. Semen samples were collected on site and testing was completed within approximately 15 minutes of liquefaction and 1 hour of collection. Test results were recorded separately in a blinded fashion between the amateur and professional operators, with results recorded on separate documents.
After completing the YO test, each amateur completed a YO usability questionnaire. The YO Usability Survey included five5 questions with five5 possible responses, for selection by study participants. The user questionnaire was based on the Likert survey principle limited to a 5-point scale providing a variety of questions and answers for selection covering the entire range of user satisfaction. Amateurs articulated their experience conducting the YO test by answering subjective questions relating to the overall procedure, preparation of the semen sample, use of the YO device, filling the slide with the sample, and the quality of the instructional animations and videos. Amateurs also rated both the clarity of instructions and how easy the directions were to follow.
Statistical Methods
Positive and negative percent agreement (PPA and NPA) calculations were used to statistically evaluate agreement of the results. This initially involved calculating agreement of the qualitative YO results between amateur and professional users (Table 2). To further validate the accuracy of the YO test, percent agreement was also calculated between amateur YO users and SQA-V results, and professional users and SQA-V results (Table 3). For statistical modeling, the SQA-V quantitative results for MSC were restated as qualitative based on the 6 m/mL cut-off.
RESULTS
The amateur group of 316 participants represented the demographic diversity of the U.S. target audience for the YO Home Sperm Test (Table 1) and encompassed a broad range of users including male donors with unknown fertility status, men with known fertility issues, and women who tested donor samples. The YO MSC result of each amateur user was compared to the YO MSC result obtained by a professional lab technician (Table 2). Overall agreement (PPA and NPA) of YO results of amateurs vs professional users was >96%, with overall accuracy >97%. The inter-site accuracy coefficients of variation of <2% demonstrate very close agreement between the three test sites.


Evaluation of the amateur participants’ responses to the YO Usability Survey showed that more than 96% found the directions and pictures in the YO test procedure very or somewhat clear, and easy, or fairly easy to follow (Fig. 1).


DISCUSSION
Although Smartphones are not yet technically able to provide a full semen analysis comparable to laboratory-automated semen analyzers, portable approaches to semen analysis make it possible for men to perform a “good quick check” that may uncover early clinical indications that further investigation is warranted.15
The need for gold standard semen analysis is not replaced, but simply supplemented by Smartphone screening or early warning technologies. Just as a “normal” semen analysis does not rule out further evaluation of the male, a YO device test result of MSC >6 million/mL does not suggest that men should forgo a formal fertility evaluation and/or additional more complete semen analysis especially if attempting to conceive for an extended period or if there are known male or female fertility risk factors present. Likewise, if the YO test result reports a MSC of <6 million/mL an evaluation by a male reproductive specialist as well as a confirmatory and more complete semen analysis is recommended. With these caveats and limitations, accurate home sperm testing may still have an impactful role in providing an initial and preliminary male fertility assessment, especially for those men in remote and resource-poor areas.16
Another benefit to home testing is home collection, which has recently been widely used to provide comprehensive semen analysis and sperm freezing services. After collection, the sample is mailed in a sperm preservative and temperature-controlled environment. This option can be expensive, and it presents challenges to preserve motility during the time required for shipping, but it has been shown to successfully report many semen parameters.
For the first time, the 2021 AUA/ASRM male infertility guidelines have clearly stated that in the presence of male factor infertility, an evaluation by a reproductive urologist is recommended to address the etiology and rule out an underlying medical disease. In more than half the cases, male infertility can be attributed to one of several medical conditions, including endocrine disorders and testicular cancer, that might otherwise remain undetected.3
Regardless of the reason for postponing a male fertility investigation, if an undiagnosed medical disease is present, subsequent treatment may be critically delayed. In these cases, an affordable, at home semen screening test or home collection mail-in option could alert an individual to the possibility of male factor infertility and motivate him to seek professional investigation sooner.
Access to a professional medical opinion via remote monitoring and testing devices already exists in many medical specialties. The COVID-19 pandemic highlighted the capabilities and enhanced the acceptance of telehealth and home testing platforms especially for nonemergency medical care such as initial fertility assessments.
For a home sperm test to be utilized and demonstrate value, it must provide reliable results when used by an amateur user. In 2018, Agarwal et al demonstrated that the YO device had a high level of accuracy and precision when compared to the automated SQA-V laboratory analyzer.6
However, this study was limited by the small number of participants (24 men), was a single-site study and lacked amateur user experience feedback.
In an effort to better define the usability of the YO device, this study analyzed clinical data and user feedback from 316 amateur participants who ran their own YO test. For this largest study to date, the participants were selected to reflect the U.S. demographics of potential YO users, and the study was conducted across three different sites from two continents.
The participants ranged in age from 18 to 59, with over 90% aged 18 to 39. Although 92% of the cohort were male, 24 women performed the YO test using a donor sample. This helped to reflect the possibility that in some couples, the female partner may perform the test on behalf of the male. The YO test must also be suitable for users of all backgrounds, and the study involved participants of white, latino, black, and asian ethnicity. Furthermore, the individual’s highest educational level was recorded to ensure that the YO test was user-friendly regardless of educational attainment or qualifications. In the amateur group, 23% of users had not attended an educational setting past high school, 62% had technical school or some college experience and just 13.6% had a postgraduate education. Reflecting the demographics of potential YO users in this study allowed conclusions to be drawn regarding whether a broad range of users could operate the YO test to obtain accurate results.
Despite our best efforts to avoid biases in the study, some limitations and shortcomings do exist. The study did not comprise “real world” consumers, but the demographics of the study population were aimed to reflect the YO target audience as closely as possible. The YO test is not a replacement for standard semen analysis. As a home screening device, it does not evaluate additional baseline semen parameters such as semen volume or sperm morphology or have the capacity to determine more advanced assessments of sperm quality such as DNA fragmentation. If the YO test appears normal and infertility persists, then proceeding to a formal laboratory semen analysis that provides all standard parameters is recommended sooner rather than later and in addition because MSC is an important parameter for assisted reproductive technologies, specifically IUI, a complete semen analysis will likely be performed prior to initiation of fertility therapy. We contest that manual SA remains the gold standard.
This study was conducted based on the still widely utilized 5th edition WHO guidelines for semen analysis. The 6th edition expanded the distribution of semen variables, providing new lower reference limits based on a study of approximately 3500 men from 12 countries and across 5 continents. The new lower reference limits of 16 m/mL sperm concentration and 42% motility (equating to an MSC of 6.7 m/mL) reflect a minimal change to the existing YO test MSC cut-off.5, 17
Newer versions of the YO test will be updated to reflect these minor changes.
Advancements in technology, combined with enhanced usability, continue to be the primary focus of the YO Home Sperm Test mission. The improved usability not only expedites early detection but also enables a more thorough screening methodology. These advancements prove especially advantageous for patients requiring clinical counsel from a urologist. Practically, it is recommended to simplify user instructions and provide additional guidance to minimize potential errors at critical testing points. Notably, YO envisions incorporating the capability to report qualitative results for a broader range of semen parameters, while also establishing a direct link between the user and an expert MD for further consultation and fertility testing.
The YO Home Sperm Test is an FDA-cleared home semen analysis device that utilizes smartphone technology to enable users to obtain an initial impression of the male fertility status. The YO Home Sperm Test accurately reports a MSC which is a more useful integrated parameter for home fertility screening than concentration alone. It is a web-based connected device that is capable of capturing a video of the semen sample for the user to view as well as send results to a health professional, thus making it a remote medical platform.
CONCLUSION
This largest study of its kind to date defining the experience of using the YO test, an at-home sperm testing technology demonstrated that amateur participants, selected to reflect real-world users, accurately assessed whether a semen sample had a low or moderate/normal MSC below and above a cut-off of 6 m/mL. YO results were also accurate when compared to a widely utilized automated semen analyzer, the SQA-V. Furthermore, the YO test instructions were reported to provide a positive user experience, making it a valuable and usable real-world home sperm screening device suitable for an initial male fertility assessment.
Data availability
Declaration of Competing Interest
No conflict.
References
- World Health Organization (WHO). International Classification of Diseases, 11th Revision (ICD-11). WHO; 2018.
-
Trends of male factor infertility, an important cause of infertility: a review of literature.
J Hum Reprod Sci. 2015; 8: 191-196
-
Diagnosis and treatment of infertility in men: AUA/ASRM guideline part I.
. 2021; 115: 54-61
-
Development of a novel home sperm test.
Hum Reprod. 2006; 21: 145-149
- WHO Laboratory Manual for the Examination and Processing of Human Semen. 6th ed. World Health Organization, 2021
-
Home sperm testing device versus laboratory sperm quality analyzer: comparison of motile sperm concentration.
Fertil Steril. 2018; 110: 1277-1284
- Laboratory Manual for the Examination and Processing of Human Semen. 5th ed. WHO, 2010
-
The use of semen parameters to identify the subfertile male in general population.
Gynecol Obstet Investig. 2005; 59: 86-91
-
Semen parameters, including WHO and strict criteria morphology in a fertile and subfertile population: an effort towards standardization of in-vivo thresholds.
Hum Reprod. 2001; 16: 1165-1171
-
Semen parameters in a fertile versus subfertile population: a need for change in the interpretation of semen testing.
Hum Reprod. 1997; 12: 987-993
-
Sperm morphology, motility and concentration in fertile and infertile men.
N Engl J Med. 2001; 345: 1388-1393
-
World Health Organization reference values for human semen characteristics.
Hum Reprod Update. 2010; 16: 231-245
-
Automation is the key to standardized semen analysis using the automated SQA-V sperm quality analyzer.
Fertil Steril. 2007; 87: 156-162
-
Double-blind prospective study comparing two automated sperm analyzers versus manual semen assessment.
J Assist Reprod Genet. 2014; 31: 35-43
-
Limits of current male fertility testing.
Fertil Steril. 2019; 111: 835-841
-
Extended semen examinations in the sixth edition of the WHO Laboratory Manual for the Examination and Processing of Human Semen: contributing to the understanding of the function of the male reproductive system.
Fertil Steril. 2022; 117: 252-257
-
Evolution of the WHO “Semen” processing manual from the first (1980) to the sixth edition (2021).
Fertil Steril. 2022; 117: 0015-0282
Article info
Publication history
Publication stage
In Press Journal Pre-Proof
Footnotes
Capsule: The YO sperm test can be used as an effective initial home screening tool to gain preliminary insight into the fertility status of the male in a real-world setting.
Funding Support: Medical Electronic Systems.
Identification
Copyright
User license
ScienceDirect
Figures
-
 Figure 1. YO Usability Survey results.
Figure 1. YO Usability Survey results.
Tables
- Table 1 Demographics of the YO Home Sperm Test Amateur User Population.
- Table 2 Accuracy of the YO Home Sperm Test Performed by Amateur versus Professional Users.
- Table 3 Accuracy of the YO Home Sperm Test Performed by Professional and Amateur Users versus an Automated Sperm Quality Analyzer (SQA-V).
Related Articles
- Editorial Comment on “An Assessment of The YO® Home Sperm Test”
Urology May 14, 2024
- The Role of Remote Diagnostics to Better Assess Uroflow Variability: Insights From Combining at Home Uroflows and Frequency Volume Charts From 19,868 Voids Using a Novel, Hand Held, Cellular Embedded Device
Urology April 25, 2024
Open Access
- The Diagnosis of Urinary Tract Infections Using a Novel At-home Testing Protocol to Enhance Telemedicine: A Retrospective Analysis
Urology January 9, 2023
- Racial Differences in Urinary Catheter Use Among Female Nursing Home Residents
Urology December 4, 2022
- Institutional Micro-Cost Comparative Analysis of Reusable vs Single-use Cystoscopes With Assessment of Environmental Footprint
Urology March 16, 2024
Open Access